This article is an excerpt from the Shortform book guide to "An American Sickness" by Elisabeth Rosenthal. Shortform has the world's best summaries and analyses of books you should be reading.
Like this article? Sign up for a free trial here .
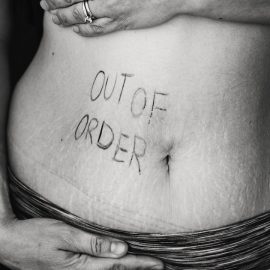
How do hospitals bill for their services? Why does hospital care cost so much more in America compared to other developed countries?
American hospital bills can get exorbitantly high because the pricing practices are designed to maximize billing to the point of what’s acceptable. Hospitals can even add optional services without necessary patient benefit—using ultrasound to inject steroids in a knee adds $300.
This article takes a look at the hospital billing system in America and gives some practical recommendations on what you can do to reduce your bill.
How Does Hospital Billing Work in the U.S.?
Hospitals provide medical service to the patient, then are reimbursed by the payers (insurers) for the service. This practice has led to a complicated set of billing practices and gamesmanship to maximize hospital earnings. Hospitals employ reimbursement consultants to adjust their prices and billing practices to earn more money.
The high sticker price given by hospitals is a negotiating point with payers (insurers). Bigger payers pay a smaller fraction of the list price than smaller payers and the uninsured.
Medicare assigns to every hospital an overall cost-to-charge ratio it considers reasonable. This is meant to constrain the profit percentage that hospitals can make. However, this regulation turned billing into a strategic game. For example, hospitals adjusted their prices to maximize billing. They lowered charges for items that are often not reimbursed (like gauze) and boosted charges for what is reimbursed (OR time, oxygen therapy).
This led to a perplexing practice where a single procedure, like an overnight stay in the hospital, can be billed separately as a wide array of items. This is why an American hospital bill can include dozens of charges, including individual Tylenol pills and charges for each separate doctor’s time.
Billing is done aggressively, to the limit of what is acceptable for the service provided. This is called “upcoding.” For example, a simple blood draw can be classified as a level 5 doctor visit.
Providers and vendors lobby to get new conditions treated as diseases since this legitimizes billing for the disease. For instance, if obesity is recognized as a disease, it gets assigned billing codes, which pressures insurers to cover it.
When new treatments appear, there is often a frenzy to promote it and set the billing standards. Because the finances of the new treatment are unpredictable and patient numbers are small, the reimbursement policy may start off being lax; this may let the cat out of the bag and make it difficult to constrain costs later.
- For example, within cancer, proton beam therapy was a new treatment option in the early 200s. Each machine was expensive, costing more than $100 million, and financing appeared to get the machines installed at hospitals. Unsure how to price the treatment, Medicare reimbursed generously. However, ultimately proton beam therapy had little proven benefit over cheaper options. The damage was already done—more machines were installed per capita in the US than in Canada and the UK, whose nationalized health services balked at the expensive treatment.
Observation Billing
Billing can cause changes in how hospitals practice care.
One example: admitting patients for “observation” means admitting them for monitoring before deciding on a treatment. Due to quirks in billing, hospitals get paid more for patients under observation. Essentially, Medicare pays bundled rates for inpatient admissions, but not for outpatient care, which observation fits under. Under observation, hospitals can charge per service as they like.
This has led to situations where patients were admitted under “observation status,” underwent a battery of tests, then were charged far more than if they had merely been admitted as an inpatient.
Charity Work
Nonprofit hospitals are required to provide “charity care and community benefit” to keep their tax-advantaged status. However, as with much of the healthcare ecosystem, this can be distorted to the hospitals’ advantage.
The ACA requires the IRS to collect each hospital’s quantitative enumeration of charitable activities and their value. Recent research suggests hospitals spend only a fraction of the tax advantage surplus on charity care—a set of 200 hospitals receive $3.3 billion in tax exemptions, but they only spend $1.4 billion on charity care.
This legal status can even open the door for political negotiations. In San Francisco, hospitals planning new construction are required to demonstrate charity care commensurate with size. For California Pacific Medical Center, Sutter Health agreed to create a $20 million Healthcare Innovation Fund, $60 million for affordable housing programs, and an agreement to not raise rates for insurers covering city employees by more than 5% annually.
What to Do About Hospital Bills
- Vet the hospital. Use these sources of information:
- US News & World Report
- Leapfrog Group on patient safety
- Medicare’s Hospital Compare program
- The New York Times’ Medicare payment database
- Look at the hospital’s IRS Form 990, the required financial reporting form for non-profits. See if they’re a hospital that compensates executives highly or earns large profits.
- As a patient in the hospital
- When admitted, you’ll be asked to accept financial responsibility for charges not covered by your insurer. Write in “as long as the providers are in my insurance network.”
- If you’re put in a private room, ask “will insurance cover this private room, or will there be a supplement fee?” If there is a fee, ask how much it is, then consider asking for a shared room with no fee.
- If staying in the hospital, ask if you are being admitted or held under observation.
- If you’re under observation, you’ll be classified as an outpatient, which means higher co-pays and deductibles.
- Ask to know the name and role of every person appearing at bedside, as well as what they’re doing. Write all this information down.
- You can refuse care from any provider. This includes less useful interactions, like the physical therapist who helps you out of bed and the dermatologist examining a harmless rash.
- Refuse equipment you don’t need.
- Dealing with bills
- Negotiate large bills. Hospitals more or less expect you to do this, which is why they have high sticker prices.
- Request complete itemization of hospital bills to see what the breakdown of costs is.
- Hospitals may insist that HIPAA or internal policy prevents this, but this is false. It’s your right to access your own healthcare information.
- If itemization takes a while and your bill goes into collection, tell the company you’re waiting for itemization and are disputing charges.
- Check the bill against your notes in hospital. Over 50% of bills contain mistakes.
- Protest bills in writing, not by phone.
- Send an email or letter, and send a copy to a local reporter, state insurance commissioner, or the consumer protection bureau.
- If the doctor’s charge is outrageous, send a copy to his national specialty’s organization.
- Compare the fees to Medicare payment rate. Use these databases to compare costs: Healthcare Bluebook, Pratter, ClearHealthCosts, FAIR Health, All Payer Claims Database.
- Argue against out-of-network bills if you didn’t provide informed consent for them.
- Reduce the costs from testing.
- Do not test outside your network.
- As a general rule, send your labs outside the hospital lab.
- Ask your commercial lab for printout of results or copy of scans.
- Avoid useless screening, such as for:
- Low back pain within the first six weeks
- Ultrasound of neck for narrowing of arteries
- Choosing Wisely, from the US Preventive Services Task Force, has a list of services that patients should question.
- However, don’t get cheap on tests that influence critical decisions (like a pathology biopsy that leads to a surgery decision).
Systemic Changes to Demand
- Require public price disclosures for every treatment and service.
- California now requires hospitals to post their chargemasters, their master list of sticker prices.
- Require hospitals to guarantee that all doctors treating you are in your insurance network.
- Your employer should insist on this during policy negotiations.
- New York law stipulates that out-of-network care during emergency room or hospital visits are not the responsibility of patient. The insurer and the hospital have to work it out between themselves.
- Encourage bundled pricing.
- This is now common for patients paying out-of-pocket. For example some centers charge $535 for a colonoscopy, with all costs included.
- It should be made more common for people paying with health insurance.
- Remove tax-exempt status from hospitals.
- Too many hospitals have questionable qualification for non-profit status. Instead, tax hospitals, then allow them to take credits or deductions when performing charity. The best hospitals will have little change, while the worst hospitals will be financially punished.
- Break up hospital conglomerates through antitrust.
- 20 years ago, FTC lost antitrust cases in healthcare
- Why? The book suggests that in this era, cooperation between hospitals was seen as a good thing.
- Also, it seems economically possible for competitors to move in and compete, which means a monopoly doesn’t exist.
- Mergers under $76 million don’t need to be reported to the FTC, but many healthcare systems make small acquisitions, so consolidation is happening under the radar.
- Recently, the trend seems to be shifting back toward more antitrust lawsuits and victories.
- Promote publicity for state Attorneys General who win a fight for patients.
- 20 years ago, FTC lost antitrust cases in healthcare
- Improve standards for billing collection.
- Insist on clear terms. When will bills be sent to collection? Six months should be the minimum time, and bills should not be sent to collections while the patient is disputing the bill.
———End of Preview———
Like what you just read? Read the rest of the world's best book summary and analysis of Elisabeth Rosenthal's "An American Sickness" at Shortform .
Here's what you'll find in our full An American Sickness summary :
- How U.S. healthcare got to the state it's in today
- Why it's so difficult to make any changes to the healthcare system
- What you can do to lower your personal healthcare costs